

Background
Healthcare mobility is a critical aspect of population movement, with significant implications for the equitable allocation of healthcare resources and the strategic planning of hospital facilities. However, the spatial and temporal characteristics of healthcare mobility remain underexplored in transport geography, particularly regarding its relationship with urban systems.
To address this gap, Prof. Zhao’s research team investigated the intercity dynamics of medical supply and demand, developing a theoretical framework for the Intercity Healthcare System (IHS) (Figure 1). Utilizing travel trajectory data from over 300 million mobile phone users, they identified nearly 2 million intercity medical visits to 1,404 tertiary-A hospitals across China. Their analysis reveals the patterns of intercity healthcare mobility among 364 cities and examines the varying roles cities play in facilitating medical travel.
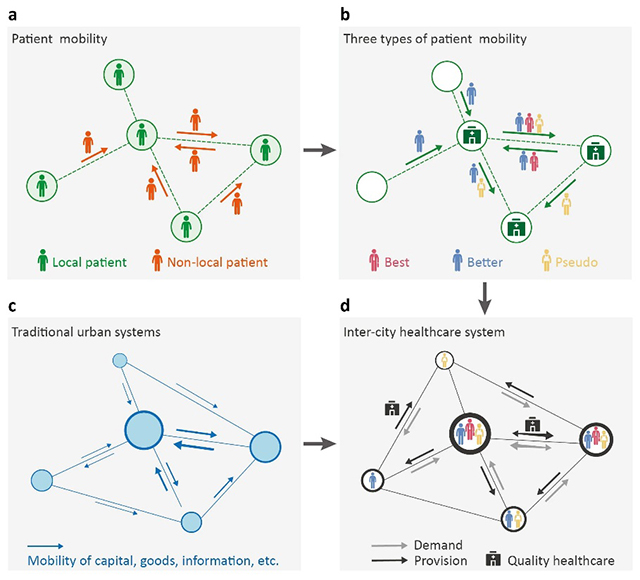
Figure 1: The theoretical framework of the ‘Intercity Healthcare System’ (IHS)
Main Findings
The study identified three types of intercity healthcare mobility (Figure 2): those seeking the best treatment (5%), who travel to top-tier medical institutions for specialized or advanced care; those seeking better treatment (76%), who opt for higher-quality healthcare services beyond their local facilities; and “pseudo” patient mobility (19%), which refers to migrants temporarily returning from large or megacities to their hometowns, where medical resources are scarce, to receive treatment.
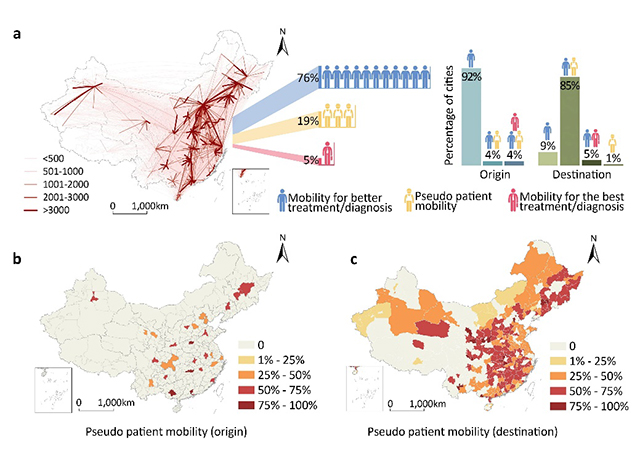
Figure 2: The pattern of intercity healthcare mobility in China
Further, bisecting K-means clustering was used to analyze the roles of cities in healthcare supply and demand. The results identified four types of supply-role cities (Figure 3): (1) National healthcare hubs (13 cities, providing 35% of the country’s cross-city healthcare services); (2) Regional healthcare hubs (30 cities, 31%); (3) “Pseudo” destinations (141 cities, 9%), where migrants return to their hometowns for treatment; and (4) Occasional healthcare destinations (89 cities, 25%). From the demand perspective, all 364 cities exhibited patient outflows, categorized into four types (Figure 4): (1) Mobile nationwide (16 cities, generating 27% of the national cross-city demand for medical treatment); (2) Mobile regionwide (33 cities, 20%); (3) Immobile (203 cities, 19%); and (4) Mobile locally (112 cities, 34%).
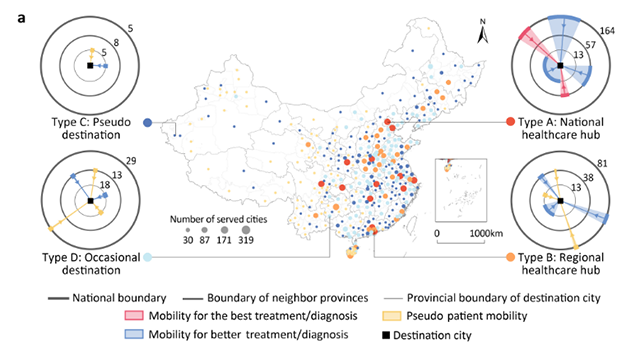
Figure 3: The supply roles of Chinese cities of IHS
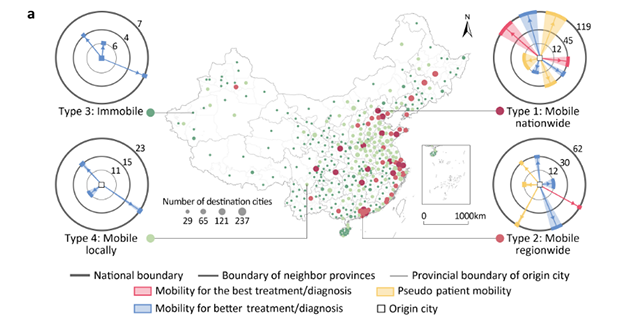
Figure 4: The demand roles of Chinese cities of IHS
The study further reveals the interdependence of healthcare supply and demand between cities through intercity healthcare mobility (Figure 5). The results indicate that regional healthcare hubs are more effective in providing high-quality healthcare services to disadvantaged mobile locally and immobile cities, which are primarily remote small and medium-sized cities, compared to national healthcare hubs. Additionally, often-overlooked occasional destination cities play a crucial role in serving the floating population from mobile nationwide and regionwide advantage cities. These advantage cities, mainly developed provincial capitals and first-tier cities, are also key destinations for migrant workers.
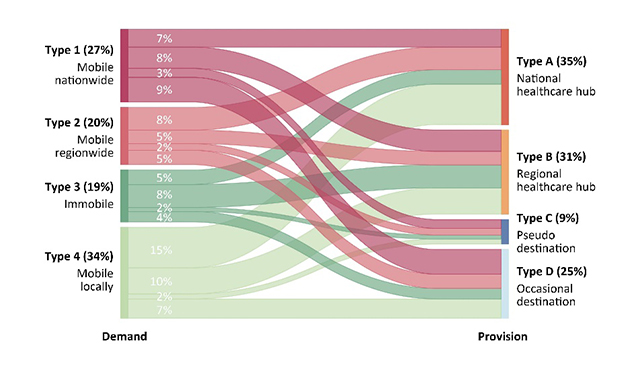
Figure 5: The interdependence of healthcare supply and demand between cities
Conclusions
The study revealed the Matthew effect in the Intercity Healthcare System (IHS), where a small number (12%) of cities with abundant local healthcare resources further strengthen their advantages by attracting additional resources through intercity healthcare mobility. In contrast, a significant portion of cities (35%) not only struggle with local healthcare resource shortages but also remain disadvantaged within the IHS, exacerbating their difficulties in providing adequate healthcare services to residents. While the IHS has helped alleviate the spatial mismatch between healthcare supply and demand, it has also introduced new structural inequalities in access to medical services. To improve equity, the study suggests enhancing the systemic status of disadvantaged cities by transforming them into more advantaged cities to promote a more balanced healthcare distribution.
Authors and Funding
The study, published in Nature Cities on January 2, 2025, is led by Prof. Pengjun Zhao as the first and corresponding author, with Juan Li as the co-first author and Mengzhu Zhang as the co-corresponding author. All authors are affiliated with Peking University.
The original paper can be accessed at https://www.nature.com/articles/s44284-024-00185-8
All figures in this report are sourced from their study.
Edited by Haochen Shi with reference to
https://mp.weixin.qq.com/s/Ppk7tW1drOGiaCwwI_fIaQ